Poster Presentation Australasian Diabetes in Pregnancy Society Annual Scientific Meeting 2016
Change in the diagnostic criteria for GDM: The Mercy Hospital for Women Experience (#106)
Background: From January 2015 RANZCOG recommended national adoption of WHO/IADPSG diagnostic criteria for GDM. Early experience from St Carlos (1) showed tripling of GDM incidence, improved pregnancy outcomes and overall cost saving.
Aim: To review the impact of change in diagnostic criteria post 2015 at a tertiary obstetric hospital in Melbourne, on the annual incidence of GDM and the rate of insulin commencement.
Method: Pathology data was obtained from 2012 to end May 2016. All POGTT performed at Austin pathology; the pathology provider to MHW were reviewed. Positive POGTT was diagnosed by a fasting glucose level ≥5.5mmol/L or a 2-hour level ≥8.0mmol/L until the end of 2014 and a fasting glucose level of ≥5.1mmol/l, and/or a 1-hour level of ≥10.0mmol/l and/or a 2-hour level of ≥8.5mmol/l from January 2015 till present. Additional cases of GDM diagnosed by external pathology providers were also recorded. Records on insulin starts were obtained from the diabetes educator log book.
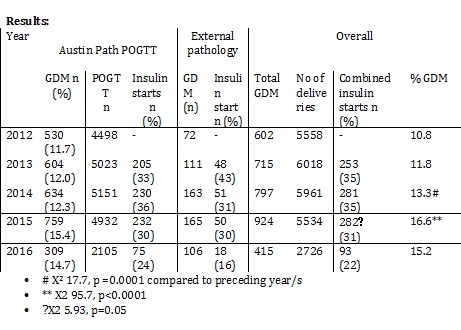
Discussion: An increase in the incidence of GDM was observed in the year prior (2014) and also again in the year following (2015) the official change. The 2014 increase may result from use of new and old criteria; pre-emptive change. The increase GDM rate to 16.6% in 2015 fell below the previous prediction of 19%(2) at our institution.
Although the absolute insulin starts did not change the percentage GDM commencing insulin decreased in 2015 suggesting that although more cases of GDM were diagnosed a greater proportion than before could be managed without insulin; i.e. milder disease. Patient characteristics, perinatal and maternal outcomes over this period are still to be assessed.
- Duran A. et al. Introduction of IADPSG criteria for the screening and diagnosis of gestational diabetes mellitus results in improved pregnancy outcomes at a lower cost in a large cohort of pregnant women: the St. Carlos Gestational Diabetes Study. Diabetes Care. 2014 Sep;37(9):2442-50. doi: 10.2337/dc14-0179. Epub 2014 Jun 19.
- Huynh J et al, Challenging the Glucose Challenge test. Aust N Z J Obstet Gynaecol 2011 Feb 7;51(1):22-5. Epub 2010 Dec 7.